Definition, Causes, Diagnosis, and Treatment for Alzheimer’s

The most prevalent type of dementia in the world, Alzheimer’s disease (AD), is a progressive neurological condition that accounts for 60–70% of all dementia cases. Despite the fact that only about 10–15% of cases are hereditary, the majority of cases are sporadic and are linked to a variety of risk factors. For Alzheimer’s disease, there is currently no cure or medication to slow the progression of the condition.
Key Symptoms: Mild cognitive impairment at first with moderate memory loss of recent events, followed by progressively severe cognitive impairment with profound amnesia, along with changes in personality, behavior, and motor function that finally result in death.
50 million individuals worldwide currently suffer from dementia, and of those cases, 6 in 10 involve Alzheimer’s disease, including 5.8 million in the US and 850,000 in the UK (as of 2018).
Onset and prognosis: Death usually happens 3–9 years following onset, which typically occurs after the age of 65.
Read more about Alzheimer’s disease here.
Alzheimer’s illness Warnings & Symptoms
the root causes of Alzheimer’s
Alzheimer’s illness Alzheimer’s Disease: Diagnosis, Treatment Options, and Prognosis
Support for People and Caretakers
How is Alzheimer’s disease defined?
Around 60% of dementia cases worldwide are caused by Alzheimer’s disease (AD), making it the most prevalent type of dementia. Alzheimer’s is a neurological condition that progresses over several years, with symptoms that gradually get worse. Like with most dementias, Alzheimer’s symptoms typically start out mild, with trouble recalling recent events, before escalating to more severe signs and symptoms over time (outlined below).
Alzheimer’s is typically an old age disease that gets more prevalent beyond the age of 65. Dementia, on the other hand, is not a natural or healthy aspect of aging. With just 5% of instances occurring in those under the age of 65, Alzheimer’s disease can very rarely afflict people who are considerably younger (between 30 and 40 years old). The causes of early-onset Alzheimer’s are typically a little different from those of sporadic Alzheimer’s disease, despite the fact that the disease is the same in both cases.
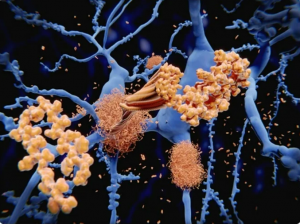
Despite the fact that the precise etiology of Alzheimer’s is still unknown, the disease is characterized by two important pathological features: amyloid plaques and tangles (discussed in detail later). These aberrant proteins cause the death of neurons over time, resulting in cortical atrophy, which causes the symptoms of Alzheimer’s and causes mortality nine years after the onset of symptoms.
Signs and symptoms of Alzheimer’s disease
Because Alzheimer’s disease is a neurological condition that progresses over time, its symptoms start out mild and modest before progressively getting worse over a number of years. Depending on the precise cause and mechanism at play, each affected person’s start, severity, and rate of development, as well as time until death, differ greatly.
Three stages can be distinguished between the signs of Alzheimer’s disease:
Symptoms in the early stages:
Subtle memory loss of recent events can manifest as forgetting a recent conversation or incident, asking the same questions repeatedly, or having trouble choosing the right words to use in conversations.
Increased worry and bewilderment can be signs of subtle behavioral or mood changes that are not normal for the individual.
Making decisions is becoming harder, and you may be more cautious about certain things, among other cognitive symptoms.
It is crucial to remember that occasionally losing things or forgetting things is a natural aspect of getting older; however, when this happens frequently, it frequently indicates dementia.
Symptoms in the Middle Stage:
deterioration of memory loss, which leads to losing the faces and identities of loved ones as well as their names
Increased nervousness, irritability, and indications of repetitive or impulsive behavior cause mood shifts to become more pronounced.
Anxiety and depressive symptoms, including lack of motivation
Delusions and hallucinations may occasionally show indications.
Sleep issues like insomnia are quite typical.
the onset of motor issues, including aphasia (speech problems)
Activities of daily life are hindered at this point, and patients typically need some amount of care and help, especially as the disease advances.
Symptoms in the late stages:
With increased distress for both the patient and caregiver, all of the aforementioned behavioral, emotional, motor, and cognitive symptoms worsen.
Patients may develop mistrust of those around them, especially loved ones, and caregivers frequently face violence.
Some individuals may experience significant weight loss due to feeding problems.
Urinary and bowel incontinence, trouble placing oneself, significantly decreased speech, and worsening motor issues are all potential side effects.
Activities of daily life are substantially hampered at this point, and patients typically need full-time care and assistance. Patients’ symptoms deteriorate and grow more reclusive, finally leading to death.
Many Americans overestimate alcohol’s link to cancer
Numerous times, things other than the pathophysiology of Alzheimer’s can accelerate the disease’s course. These include illnesses including delirium, infections, and strokes. The signs of dementia might occasionally get worse when taking certain drugs. The average time between the onset of symptoms and death is 3 to 9 years.
The signs of dementia in general and Alzheimer’s disease are very similar. The pathology and symptoms of vascular dementia, which frequently begins with more severe motor impairment, are also frequently seen by Alzheimer’s patients over the age of 65.
the root causes of Alzheimer’s
The majority of sporadic occurrences of Alzheimer’s have an underlying etiology that is still poorly understood, while 5–10% of cases can be attributed to genetic variations that are now well understood.
Genetics
Familial Alzheimer’s disease, which affects 5–10% of cases overall, is brought on by inherited genetic changes to important genes. Autosomal dominant inheritance, which causes early-onset Alzheimer’s before age 65 in less than 1% of all cases of the disease, is unusual (rare).
The three major deterministic genes (directly causative) APP, PSEN1 and PSEN2 are linked to hereditary types of Alzheimer’s. These genes work together to process amyloid and create beta-amyloid plaques, the primary pathogenic feature of Alzheimer’s disease.
Because of this, having a family history of dementia may indicate that particular genetic abnormalities exist in the family gene pool and that you may be at a higher risk of acquiring Alzheimer’s. If this is the case, genetic testing and counseling might be provided.
Several risk genes have been linked to Alzheimer’s, albeit their causality has not been established. The most prevalent of these genes is the APOE4 allele, which, depending on how the APOE4 alleles are inherited, raises the risk of Alzheimer’s disease by 3–15 times. According to estimates, at least one APOE4 allele is present in 60% of all Alzheimer’s patients. The severity and development of the disease may be aggravated by having APOE4 alleles in addition to other deterministic genes, other risk factors (listed below), or both.
Autosomal dominant variations in the genes ABCA7 and SORL1 are also involved. A three times increased risk of developing Alzheimer’s disease is also believed to be associated with allelic variants of TREM2 (microglia involved). There are several polymorphisms (minor genetic variations; SNPs) in up to 20 more genes that are linked to an elevated risk of Alzheimer’s disease.
danger signs (Protective & Destructive)
Although there are multiple significant risk factors involved, the specific method by which Alzheimer’s disease develops is still poorly known, aside from its genetic causes.
Factors that raise the likelihood of developing Alzheimer’s include:
The chance of having Alzheimer’s increases every five years after age 65, and 1 in 6 people over the age of 80 have dementia.
Head injuries – A link has been shown between serious head traumas and the onset of Alzheimer’s. Furthermore, dementia symptoms and prognosis may worsen if a person has head injuries.
Cardiovascular disease – Lifestyle choices that increase the risk of heart disease include diabetes, high blood pressure, high cholesterol, smoking, and obesity. These variables are also linked to an increased risk of vascular dementia (primarily) and Alzheimer’s disease.
Down’s syndrome – Trisomy 21 is the genetic cause of Down’s syndrome, which has a third copy of chromosome 21 and an extra copy of the APP gene, which makes beta-amyloid. A 50% increase in amyloid formation over baseline levels results from having an extra copy of the APP gene. As a result, those who have Down syndrome have an increased risk of getting Alzheimer’s.
Sedentary lifestyle, hearing loss, stress, and untreated depression are some more prevalent risk factors that may help someone develop Alzheimer’s disease.
Additionally, a single study has linked calcium supplementation to Alzheimer’s disease, but only in older women with a history of stroke.
As was already indicated, the vast majority of the time, dementia is not an inevitable byproduct of getting older, and you can actively lower your risk of getting Alzheimer’s and other dementias. Your risk can be decreased by a variety of active lifestyle choices. These comprise:
By giving up smoking, leading an active, non-sedentary lifestyle, decreasing weight if you’re overweight, eating a healthy, balanced diet rich in fresh fruits and vegetables, and consuming less alcohol, you can lower your chance of developing cardiovascular disease.
Maintain a healthy medication regimen and adopt active lifestyle modifications, such as controlling your blood pressure and blood sugar levels, if you have diabetes.
Keeping your mind active, even if it’s only reading, solving crossword puzzles, or playing Sudoku.
Short-term cognitive improvement from playing brain training games is useful.
Participating in team sports or volunteering in your community is advantageous because loneliness and social isolation can also raise your risk of dementia.
Alzheimer’s Disease’s Effects on the Brain
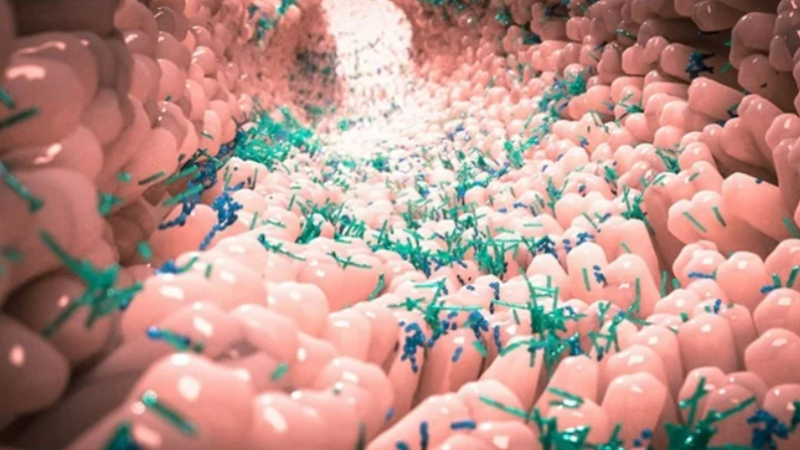
The two primary pathology indicators of Alzheimer’s disease are beta-amyloid plaques, which develop in brain tissue and around blood vessels (cerebral amyloid angiopathy), and tau protein tangles within neurons. All of these work together to cause neurodegeneration (death of neurons and synaptic connections), which causes general brain atrophy (shrinkage) in the cortex and hippocampus. The intensity of symptoms and the development of the illness are correlated with neuronal death and atrophy in significant brain areas.
The many kinds of dementia share a lot of clinical and pathological similarities. Alzheimer’s patients’ brains can occasionally include Lewy bodies of alpha-synuclein, the main protein involved in Parkinson’s disease and dementia with Lewy Bodies. Atherosclerosis, which is the buildup of fatty plaques inside the brain’s blood vessels, can also result in vascular dementia and stroke. Additionally, Alzheimer’s patients may have TDP-43 (a critical protein associated with motor neuron degeneration) in their brains. Mixed dementia is the concomitant occurrence of two or more dementias, with Alzheimer’s disease and vascular dementia constituting the most typical mixed dementia.
It is now understood that up to one-third of all cases of Alzheimer’s thought to affect those over 85 years old may not actually have the disease at all. Older people who have a dementia known as limbic-predominant age-related TDP-43 encephalopathy, or LATE, experience symptoms that are very similar to those of Alzheimer’s disease but are brought on by the TDP-43 protein rather than amyloid. This finding has significant ramifications for the proper diagnosis, therapeutic approaches, prognosis, and researchers looking into the causes and possible treatments for Alzheimer’s disease.
Alzheimer’s illness Diagnosis
It is possible to overlook or blame drugs, stress, depression, or anxiety, which can mimic AD, for short-term memory loss or mild, early signs of dementia. However, if these symptoms continue to progressively get worse over time, it could indicate dementia.
Unfortunately, there is no one test that can accurately diagnose Alzheimer’s or any other kind of dementia. Your general practitioner (GP) may recommend you to a specialist, typically a neurologist and/or psychiatrist in a specialised memory clinic, if they are concerned that the symptoms could be caused by dementia. A neurologist will check for dementia’s physical symptoms, while a psychiatrist will look at the condition’s cognitive symptoms. A CT or MRI scan of the brain may be suggested by a neurologist in order to evaluate any brain abnormalities and confirm or rule out a diagnosis.
Cognitive ability is evaluated at the memory clinic using a standardized questionnaire known as the short mental state examination (MMSE). A score of more than 24 on these 30 questions shows normal cognitive function. Typically, scores between 19 and 23 are categorized as mild cognitive impairment, 10 to 18 as moderate cognitive impairment, and 9 or below as severe cognitive impairment. These results must be modified for age and educational level, though.
The MMSE, brain imaging, and exclusion of other explanations (such as by blood testing for pharmaceutical interactions) all work together to help make a favorable diagnosis. Because the early signs are so mild, this may take some time. The diagnosis could grow simpler as the illness worsens, though.
Alzheimer’s Disease: Treatment Options & Prognosis
At this time, neither a cure nor significant disease-modifying treatments exist for Alzheimer’s disease. There are, however, many drugs that can momentarily reduce discomfort.
Existing Medications
Acetylcholinesterase (AChE) Inhibitors: Acetylcholine, a crucial neurotransmitter, is hypothesized to be diminished in Alzheimer’s disease. Acetylcholine’s levels in the brain are raised as a result of AChE inhibitors’ ability to stop its breakdown. They consist of donepezil and rivastigmine.
Glutamate Inhibitors, such memantine, SSRI-based antidepressants, and antipsychotics, like risperidone
None of these drugs address the pathology or underlying reasons of the disorder; instead, they just manage some of the symptoms. With the use of drugs for diabetes, high blood pressure, high cholesterol (such statins), and cardiac issues, underlying cardiovascular disease and associated risk factors can be changed (such as aspirin).
Alternative Treatments
Cognitive rehabilitation – with the help of a skilled therapist and caregiver, individuals can gradually accomplish personal goals like carrying out daily duties.
Cognitive Participating in social or group activities that stimulate the mind and hone problem-solving and memory abilities
Reminiscence is the active recall of former experiences with the aid of visual (such as pictures) and auditory (such as music) aids. As a result, mood and wellbeing may improve.
Additionally, it has been demonstrated that listening to old music can uplift mood and behavior and revive long-forgotten memories (calming effect). Additionally, it has lessened social isolation and promoted social engagement as well as the expression of emotions.
Symptoms are only momentarily relieved, and the illness course will eventually deteriorate, much like with pharmaceuticals, which may be combined with non-medication alternatives.
Alternative Medicine and Prevention
Although there isn’t enough proof to support their efficacy, a variety of complementary therapies are thought to benefit dementia patients. Here are a few of these:
Coconut oil Bright Light Therapy (to alleviate insomnia in Alzheimer’s disease) Turmeric (Curcumin)
Although the efficacy of these supplements has not yet been thoroughly established, moderate use of them typically has no negative effects. Like with most alternative medications, the bulk of extensive research do not appear to indicate any appreciable effects of such drugs on the effective management of medical disorders. Patients and caregivers should not choose alternative medicines above traditional drugs and therapies when contemplating alternative medications.
Clinical Trials Being Done Now
There are a number of important clinical trials that are ongoing with the intention of examining the effects of various treatments:
Sargramostim – decreases beta-amyloid buildup
Selective inhibitors of beta-secretase, MK8931 (reduced production of amyloid)
CAD106 – promotes beta-amyloid immunity without inducing an autoimmune reaction
Inhibits the buildup of tau is TRx0237.
Improvement of blood sugar regulation and insulin resistance in the brain with intranasal insulin
We still don’t know how well these treatments will work to change the course of the disease and dramatically lessen symptoms.
Support for People and Caretakers
Receiving a dementia diagnosis can be challenging and stressful for the person receiving it as well as their close relatives and friends. To the contrary, there are numerous exemplary organizations that provide assistance to patients and carers.
Both Alzheimer’s Research UK and the Alzheimer’s Society are located in the UK. There is the Alzheimer’s Foundation of America and the Alzheimer’s Association in the US. Additionally, there are global organizations like Alzheimer’s Disease International. Their websites offer a wealth of resources for finding support services as well as additional information on the disease.