The Microbiome and Alzheimer’s Disease
The microbiome: What is it?
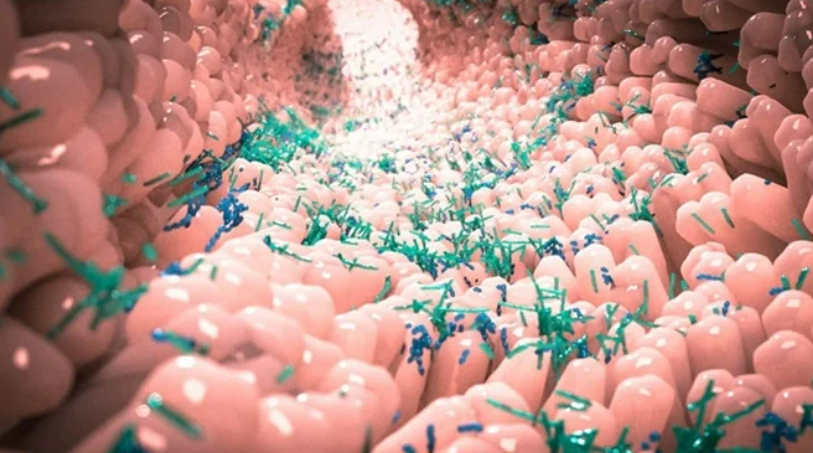
In comparison to the number of human cells, our bodies contain more than ten times as many bacteria and other microbes. Microorganisms such as bacteria, viruses, fungi, and others live in the gastrointestinal tract, particularly in the intestines, and are essential to the health of the digestive and immune systems.
The ‘good bacteria’ that make up the majority of the microorganisms live in harmony with the host. The quantity of “good bacteria” in the gut can be increased and maintained by following a healthy diet and an active lifestyle. However, “bad bacteria” may undermine these colonies, causing dysbiosis (an imbalance in the gut flora) that can result in a variety of health issues, from inflammation to colorectal cancer.
The overuse or misuse of antibiotics, loss of sleep, increased stress levels, excessive alcohol consumption, a lack of “prebiotics” like fiber foods, nuts, and lentils, as well as failing to eat a varied, healthy diet can all promote the growth of “bad bacteria.”
Alzheimer’s disease and the microbiome
Early Pregnancy Symptoms
The enteric nervous system is made up of approximately 500 million neurons in the gut (ENS). The “gut-brain axis” is the term used to describe how the digestive system affects and interacts with the nervous system, and vice versa. Numerous pieces of recent data point to the possibility that the gut-brain axis has a role in a number of neurological conditions, such as multiple sclerosis (MS), Parkinson’s disease, and dementia.
According to a recent study, patients with Alzheimer’s disease have different gut bacterial compositions than healthy controls. As an illustration, Alzheimer’s patients had lower concentrations of Clostridium and Bifidobacterium species, whereas Bacteroides and Gemella were more prevalent.
Additionally, alterations in the number of certain bacteria in the gut may be linked to changes in the amounts of cerebrospinal fluid (CSF) indicators for Alzheimer’s disease, such as the levels of amyloid-beta protein. For instance, there may be a clear correlation between low levels of Bifidobacterium (which is known to be reduced in Alzheimer’s) and high amounts of amyloid-beta-42 (A-42) in the CSF of Alzheimer’s patients. The level of pathogenic indicators in the CSF increases in proportion to the difference in gut bacterial levels.
How do various bacteria affect the stomach and the brain? Needed research on specific bacterial families to uncover viable explanations for this baffling question. For instance, obese mice fed a high-fat diet frequently have certain cognitive deficiencies, but when given the bacterium L. helveticus R0052, their symptoms and inflammation caused by excess weight are improved.
How Webinars Can Help You Boost Lead Quality
On the other hand, certain microbes can promote and cause inflammation via the gut-brain axis. Bacteria that produce amyloid and lipopolysaccharides (LPS) can cause severe inflammation in the gut, which then affects the brain. In addition to making the blood-brain barrier (BBB) more permeable, inflammation in the gut can make it “leaky.” Therefore, a damaged BBB allows inflammatory chemicals to enter the brain and cause brain inflammation, which may lead to or hasten the pathogenesis of Alzheimer’s disease. Bacteroides fragilis is one such bacterium that may cause neuroinflammation and hence start neurodegeneration through the gut.
Treatment and Prevention of Alzheimer’s
A growing body of recent research indicates that the gut-brain axis may have a role in the development of Alzheimer’s disease as well as widespread neuroinflammation caused by unbalanced gut microbiota (dysbiosis). Promoting “good bacteria” in the stomach in contrast to “bad bacteria” may be crucial for preserving neurological, immunological, and digestive health.
A healthy balance of gut microbiota is naturally promoted by fresh plant-based foods, probiotics in yogurt, and prebiotics in the diet. Fruits, vegetables, onions, garlic, almonds, lentils, high-fiber meals, and polyphenols (such as those found in green or black tea) are just a few examples of these. These meals may boost bacteria like Prevotella while reducing the number of Bacteroides. Gut-mediated neuroinflammation should be prevented by maintaining optimal gut health. These items are abundant in the Mediterranean diet, which has been found to lower the risk of dementia as well as heart disease, diabetes, and cancer.
Our knowledge of how specific gut bacteria can affect brain health is still in its early stages. For instance, studies have demonstrated that giving specific mice Bifidobacterium may enhance cognition. But before any research on the gut flora leads to efficient treatments for Alzheimer’s disease, much more effort is required.
Given the high correlation between gut microbiota and brain health that has so far been demonstrated (particularly in relation to Alzheimer’s disease), this area of therapeutic study may one day prove to be very important.